Wound care technology brings benefits for HME providers & patients
Thursday, November 14, 2019
This year marks the 50th anniversary of the development of air fluidized therapy (AFT) or Group 3 beds. Although the beds have been used successfully in treating nonhealing Stage 3 and Stage 4 pressure wounds in institutional settings, few home medical equipment (HME) dealers are aware of their benefits for home use.
AFT beds are seen by wound care specialists as the “gold standard” in providing patients the best possible pressure relief. Medicare and other insurers cover the bed (HCPCS E0194) if a patient has a nonhealing Stage 3 or Stage 4 pressure wound on the trunk or pelvis and previously failed a Group 2 surface. Depending on the state of service, Medicare reimburses between $3,184 and $3,746 per month for the AFT bed or the E0194 code.
These beds will allow your company to take on the most difficult pressure wound patients and provide your home health customers with solutions for their worst wound patients. Discharge planners in hospitals view these beds as a possible solution to their frequent flyer wound patients, who often have recurring admittances into hospitals.
Jennifer Orr, vice president of Medical Modalities in Concord, North Carolina, said that AFT beds are a big part of their marketing strategy.
“AFT beds have allowed Medical Modalities the ability to accept and care for the most complex wound patients,” she said. “By coupling negative pressure wound therapy and support surfaces, we truly believe that we have the most comprehensive offering of wound care solutions throughout the continuum of advanced wound healing.”
How AFT Works
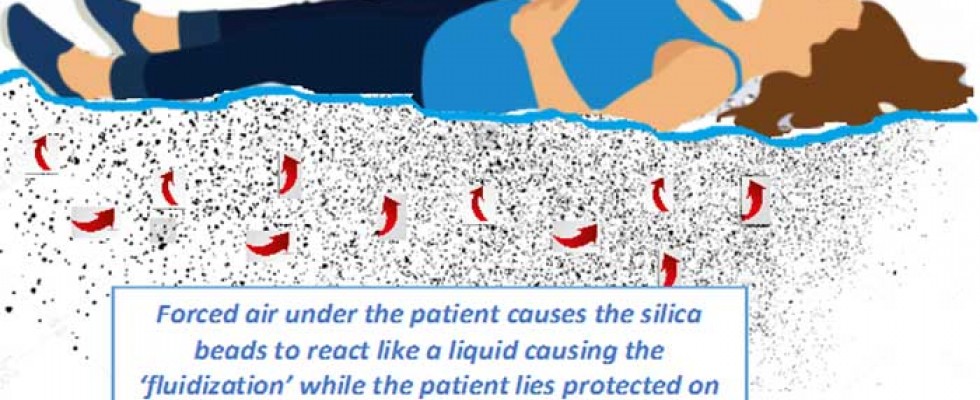
AFT beds are filled with tiny silica—or glass—beads, called microspheres, which are covered with silicone and resemble white sand. When blowers under the beads are activated and the air is forced through a porous diffuser board, the beads react like a liquid in a process called fluidization. Patients are protected from the beads by a filter sheet and lie on top of a waterproof sheet that reduces shearing and friction as well as moisture buildup. As patients lie on the waterproof sheet, they sink into the beads, which reduces pressure. Pressure is the enemy of patients with severe Stage 3 and Stage 4 pressure wounds, and when the pressure gets too high, it prevents blood flow from entering the wound site. Capillary closure, the point at which blood flow stops, occurs somewhere around 32 millimeters of mercury (mmHg) on most people. However, patients lying on an AFT surface typically have their highest pressure registering in the low teens of mmHg—thus allowing blood flow to areas that would otherwise be restricted.Value of a Home Survey
Because patients are expected to lie on AFT beds for at least 16 hours per day, a home survey should be completed before delivery. Providing a home visit accomplishes two functions: First, it ensures that the home has adequate flooring and electrical sourcing to support the bed; second, it encourages the patient’s compliant use of the bed. Although the bed requires only a standard 110-120 volt outlet, the chosen outlet must be grounded and dedicated only to the bed. Setting expectations for use of the bed with both patients and caregivers is critical. Patients need to commit to lying on the bed for at least 16 hours daily. It may help to remind them that every therapy tried to this point has been unsuccessful and that the dealer requires this commitment. Fortunately, healing occurs relatively quickly, and in a month’s time nurses should report a significant reduction in the patient’s wound or wounds. Obviously, nutrition and other factors play into wound healing, but home health nurses see positive results in patients using the AFT bed who have been classified as lost causes. Once the wounds are completely healed, patients are able to return to their original routine.Staffing & Service Requirements
The AFT bed is designed as a hybrid bed to service both institutional and homecare patients and is built with a modular design, which allows beds to be built into the patient’s convalescent room. One model of AFT bed for home use has two base pedestals that hold the bed’s tub weigh only 228 pounds. The 900 pounds of microsphere beads make up most of the bed’s weight; they are brought into the home on a dolly with pneumatic wheels. Setup can be completed in about 45 minutes. A dealer should have a van and two technicians for delivery. A patient lifter and trapeze bar and base are often ordered with the bed to facilitate patient transfer. Patients can remain on the AFT bed until healed (an average of five months). Once the patient is healed, the service team dismantles the bed wearing protective gloves and returns it to the shop to be disinfected. Beads can be disinfected after each patient and placed in a decontamination cooker that raises temperatures high enough to sanitize the beads for future use. The bead decontamination unit is about 4’ x 3’ x 4’ and sits on five-inch casters that allow it to moved out of the way when not in use. The bed is serviced by accessing the electrical components at the foot of the bed so as to not disturb the patient. Components are designed to be plug-and-play, so repairs can be done at the patient’s home and do not require a complete replacement of the existing bed.Why AFT Beds are Relevant
Reimbursement for Group 2 surfaces (primarily E0277) is only around $200 per month, so dealers are providing inexpensive solutions for these patients. Conversely, AFT beds are not part of competitive bidding, making it attractive for new dealers to provide this needed therapy. Increasingly, HME dealers have seen a trend of more debilitated patients being sent home from institutional settings. With the new Patient-Driven Payment Model (PDPM) in nursing homes and the Patient Driven Grouping Model (PDGM) in home health, it is unclear whether more severe wound patients will be referred for home services. Regardless, even 50 years after their development, AFT beds stand as a possible solution to take on even the most difficult pressure wound patients.Howie Morrison has been in HME since the late 1970s and owned an HME company for 19 years before selling it in 2005. Morrison formed Aurora MFG with Rick Fisher and Gene Gregory in 2006 to develop and promote the HydroAire air fluidized therapy bed.
