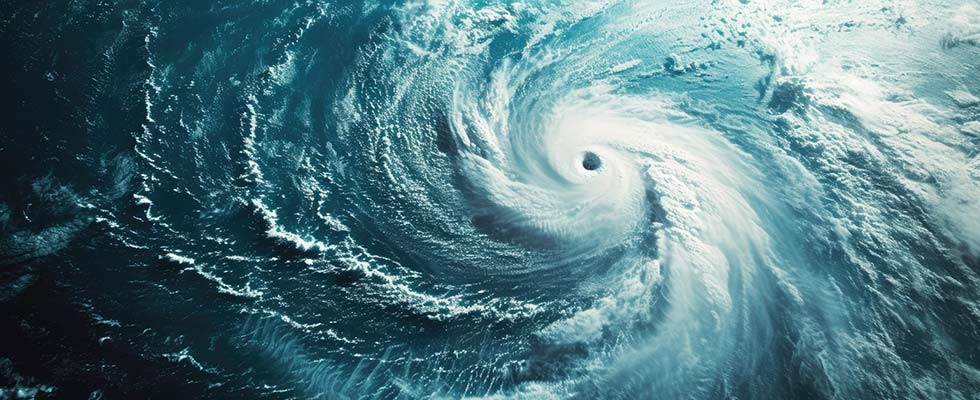
When hurricanes approach, in-home care organizations face challenges that are vastly different from those of facility-based providers. In addition to safeguarding infrastructure, we must ensure the safety of mobile care teams, maintain critical supply routes and coordinate services for patients whose needs don’t pause for the weather.
At Empath Health, we care for more than 75,000 patients annually across 20 Florida counties through hospice, home health, palliative and supportive care programs. Our teams aren’t centralized—they’re on the road, in homes and dispersed across regions that may be affected in very different ways by the same storm. Over the years, we’ve learned that effective hurricane response in home-based care depends on three things: preparation, coordination and flexibility.
Start With People
In May, before hurricane season begins, we launch a systemwide campaign focused on colleague readiness. Whether delivering oxygen, providing end-of-life care or supporting a recent hospital discharge, we must know where our team members are, how to reach them and what their storm plans include.
All staff are required to verify their contact information, report their evacuation plans and identify backup communication methods. We encourage team members to evacuate within our service area when possible so they can return to work quickly and safely after the storm.
We also use AlertMedia to issue real-time, location-specific updates to both personal and work-issued devices. Whether the message is about shifting routes, unsafe areas or suspended visits, speed and clarity of communication keep our teams protected and aligned.
Map Access Before You Need It
As forecasts take shape, we shift our focus to continuity of care. We identify patients with oxygen, IV or equipment needs—especially those who are mobility-limited or without a reliable caregiver. Then we prioritize equipment drops, medication deliveries and pre-storm check-ins based on urgency and geography.
Our durable medical equipment (DME) and logistics teams are embedded in this clinical planning process. We pre-position backup oxygen, prepare non-electric options when possible and assign mobile techs to zones based on anticipated impact.
Last year, when Hurricane Milton struck, our affiliate in Ocala, Empath Hospice of Marion County, delivered 200 oxygen tanks to Clearwater and deployed technicians multiple times in the weeks that followed to help stabilize operations. That kind of cross-region coordination isn’t a luxury—it’s essential.
Balance Protocol With Flexibility
An emergency operations plan needs structure, but not rigidity. We build ours to withstand change.
That means rotating staff shifts, designating clinical leads by region and assigning “mission support” roles to non-clinical staff—whether it’s running a supply depot or staffing a communication line. Teams know their roles, escalation paths and how to switch gears as conditions evolve.
Recovery planning begins before the storm ends. Within hours of landfall, we begin wellness checks for staff and patients, evaluate transportation routes and adjust staffing to meet the most pressing needs. Those first 24–72 hours post-storm are when good planning delivers real impact.
Action Items for Your Team
If you’re leading a home-based care organization, here are a few essential practices to consider:
- Segment your patient population by acuity and mobility. Know who will need contact or care within 24 hours of landfall.
- Designate a single platform for emergency updates and build a communication chain that includes leadership, field staff and community partners.
- Integrate your durable medical equipment (DME) providers into planning conversations early. Ensure techs have delivery priorities and alternate drop-off sites mapped in advance.
- Conduct a post-storm debrief with leadership. Capture what worked, what didn’t and how you can improve before the next storm.
One Team, One Mission
Home-based care depends on trust—and that trust is tested when a storm threatens your region. Patients and families need to know someone will be there. Caregivers need to know their safety is a priority.
At Empath Health, we’ve built a statewide system that supports collaboration across hospice, home health and DME services. But no matter your size, the core principles remain the same: prepare early, communicate clearly and support your people—so they can support your patients.
Matthew P. Chaloux is the vice resident of mission care and support centers at Empath Health. He oversees facility operations, emergency management, life safety compliance, construction services and logistics across the organization’s statewide footprint. Since joining Empath in 2021, Chaloux has helped lead enterprise readiness efforts, including hurricane response and recovery. He holds an MBA from Lynn University, a bachelor’s degree from Southern Connecticut State University and Federal Emergency Management Agency certifications in emergency management. Visit empathhealth.org.
