In an effort to keep pace in the dynamic DMEPOS industry, suppliers must regularly recalibrate their business plans and operations to address the increasing challenges of supplying patients with medically necessary items and services. While contemplating potential operational modifications, a number of suppliers have voiced concerns about the impact of Medicare’s competitive bidding rules on their ability to use an Advance Beneficiary Notice of Noncoverage (ABN). With the Medicare landscape continuing to shift beneath DMEPOS suppliers’ feet, this article is intended to address some of the concepts that are fundamental to ABN usage, and particularly issues related to using ABNs in the context of the competitive bidding program. Numbered references can be found at www.homecaremag.com.
Overview of ABNs
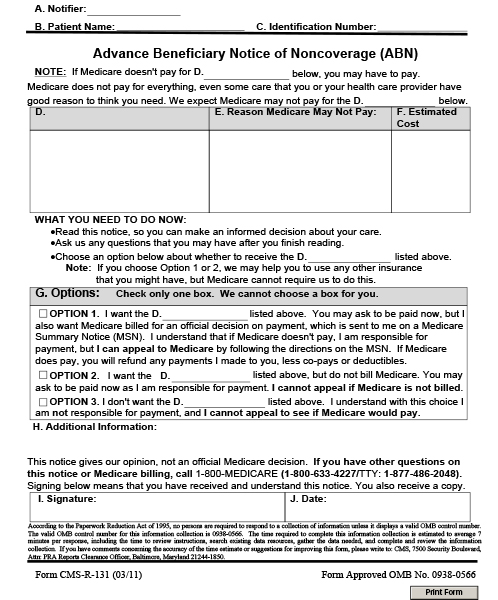 In general, the purpose of an ABN is to provide advance notice to a beneficiary that Medicare will not, or probably will not, pay for a particular item or service.1 The failure of a provider to issue a timely and properly documented ABN will subject the provider to financial liability for the services or items in question.2 In addition to publishing specific documentation standards for issuing valid ABNs to Medicare beneficiaries, such as the prohibition against using blank or routine ABNs,3 CMS has described the various circumstances in which ABN usage is mandatory and other situations in which an ABN may be issued voluntarily.4
In general, the purpose of an ABN is to provide advance notice to a beneficiary that Medicare will not, or probably will not, pay for a particular item or service.1 The failure of a provider to issue a timely and properly documented ABN will subject the provider to financial liability for the services or items in question.2 In addition to publishing specific documentation standards for issuing valid ABNs to Medicare beneficiaries, such as the prohibition against using blank or routine ABNs,3 CMS has described the various circumstances in which ABN usage is mandatory and other situations in which an ABN may be issued voluntarily.4
While federal regulations clearly state that implementation of the competitive bidding program “does not preclude the use of an advanced beneficiary notice.”5 CMS guidance provides a framework for issuing ABNs under competitive bidding. In recent months, DMEPOS suppliers have raised important questions related to whether ABN usage may or may not be appropriate. The majority of these inquiries can fit within four basic categories: 1) Upgrade ABNs for items having different HCPCS codes; 2) Upgrade ABNs for items within a common HCPCS code; 3) ABN usage and competitive bidding’s non-discrimination provision; and 4) ABN usage for non-contract suppliers within a competitive bidding area.
HCPCS Codes
CMS defines an upgrade as “an item with features that go beyond what is medically necessary,” including features that are “more extensive and/or more expensive” than what Medicare has determined to be reasonable and necessary for the patient.6 Although this definition has limits, as we will explore later, the broad language used by CMS seemingly allows suppliers to issue ABNs for nearly any excess component that may be added to a medically necessary DMEPOS item.
The use of upgrade ABNs within the competitive bidding program was addressed in a December 2010 CMS competitive bidding program fact sheet, which stated that “when a [contract or non-contract] DMEPOS supplier expects that a DMEPOS item does [not] or may not meet Medicare’s reasonable and necessary rules, it is the responsibility of the supplier to notify the beneficiary in writing via an ABN.”7 For purposes of illustration, consider the following scenario that CMS offered as an example of appropriate ABN usage within the competitive bidding program:
A physician orders a wheelchair with fixed leg rests, yet pursuant to the beneficiary’s request, the supplier furnishes medically unnecessary swing away elevating leg rests. In order for the supplier to charge the beneficiary for the additional costs associated with the upgraded item, the beneficiary must have signed a valid ABN.8
This illustration appears to clearly demonstrate that a supplier’s issuance of a properly executed ABN entitles the supplier to collect, directly from the patient, the difference in cost (the two retail charges) between the medically necessary item and the upgrade that the patient has requested. Along these lines, another viable example of an acceptable upgrade under competitive bidding would result when a beneficiary selects a not medically necessary, total electric hospital bed over a lesser model for which they qualify. Importantly, CMS specifically prohibits the use of an ABN for the purpose of substituting “one item for a totally different item (e.g., for a wheelchair when a walker was prescribed).”9 Therefore, as long as the item provided is not “totally different” than the item prescribed, when a beneficiary seeks to obtain a more expensive additional feature or an excess component that is not medically necessary, a supplier can and should obtain an ABN for the upgraded product.
“Upgraded” DMEPOS Items
In April 2007, CMS revised its Medicare Claims Processing Manual by introducing a change in its position related to the question of what constitutes a DMEPOS upgrade.10 Specifically, CMS indicated that “when an upgrade is within a single code the upgraded item must include features that exceed the official code descriptor for that item.”11 In September 2012, CMS enhanced its interpretation and enforcement of this upgrade provision by expressly stating that “DME upgrades involve situations in which the upgraded item or component has a different [HCPCS] code than the item that will be covered by Medicare.”12 Under this strengthened guidance, if a DMEPOS item does not “exceed the HCPCS code description,” a supplier appears to be prohibited from issuing an ABN to shift financial liability to a patient when the “upgrade” is merely for a “better” or “higher quality” DME item that remains within the same HCPCS code.13
Although there are valid concerns as to the operational impact of CMS’s position, which seems to challenge the traditional belief that an “upgrade” is any feature that goes “beyond what is medically necessary,”14 CMS and the DME MACs have begun to more strictly apply the Medicare Claims Processing Manual guidance for evaluating whether additional features actually exceed the HCPCS code descriptor to qualify as a true upgrade. This strict approach is and will continue to be particularly troublesome for suppliers that seek to offer upgraded DMEPOS items within a single HCPCS code that uses vague or all-encompassing code description language.
In addition to the policy and enforcement activities assumed by CMS and the DME MACs, the Medicare Pricing, Data Analysis and Coding (PDAC) contractor has also taken a more active role by broadening the scope of certain HCPCS code descriptors. As an example, beginning Jan. 1, 2013, the PDAC announced a change in the HCPCS code narrative description for Mastectomy Bras (HCPCS L8000).15 Prior to this update, code L8000 was described as a “Breast Prosthesis, Mastectomy Bra”; however, under the new narrative, code L8000 is now described as a “Breast Prosthesis, Mastectomy Bra, without integrated breast prosthesis form, any size, any type.”16 Given this revised, all-encompassing language, a mastectomy bra supplier is likely prohibited from utilizing an upgrade ABN to charge a Medicare beneficiary for the beneficiary’s request to obtain an item with more costly features such as a built-in comfort strap or specialty fabric or style enhancements. The advent of this new rule and the possibility that the PDAC will modify the narratives of other HCPCS codes may result in suppliers being forced out of the business of accepting Medicare assignment for items where upgrade ABNs are no longer available. The financial inability of suppliers to accept assignment is likely to lead to the unintended consequence of patients having to pay the full price of certain DMEPOS items out of pocket and seeking direct reimbursement for 80 percent of the allowable Medicare rate.
Discrimination Provision
Although current ABN guidance imposes a limitation on a supplier’s ability to issue upgrade ABNs for items within a common HCPCS code, CMS has not globally mandated that suppliers make each item within its DMEPOS inventory available to Medicare beneficiaries. In fact, under CMS regulations that govern traditional Medicare fee-for-service, suppliers are not prohibited from offering “good/better/best” options of DMEPOS items to patients, nor are suppliers prohibited from classifying certain items as “cash only.” CMS does not require a supplier to offer all goods to all patients, particularly in the event that such a sale would result in the supplier’s certain financial loss due to below market value third-party payer reimbursement.
However, the same cannot be said for DMEPOS items sold within a competitive bidding area. A supplier who is awarded a contract under the competitive bidding program must agree to furnish each of the items listed within its contract category to all Medicare beneficiaries who reside in or visit the competitive bidding area.17 Additionally, 42 CFR § 414.422(c) states that “items furnished by a contract supplier … must be the same items that the contract supplier makes available to other customers.”18 In contrast to CMS’s silence on this subject for traditional Medicare fee-for-service, the so-called “nondiscrimination” provision under competitive bidding expressly prohibits contract suppliers within a competitive bidding area from designating certain items as “Medicare-eligible” and other items as “cash only.”
According to CMS, the rationale for expressly including a non-discrimination provision for competitive bidding is that it “believe[s] that the inclusion of the [nondiscrimination clause within each contract awarded] will ensure that beneficiaries who obtain items under a competitive bidding program have access to the same products as other Medicare customers and private pay individuals.”19
While the non-discrimination clause is particularly relevant to contracted providers, and most notably upgrades within a single HCPCS, it does not mandate that contracted suppliers provide medically “unnecessary” equipment or components to Medicare beneficiaries without cost. The ability of DMEPOS suppliers to differentiate between medically necessary and medically unnecessary levels of service and components will distinguish the delivery as a legitimate upgrade via an ABN, or as a contract violation.
Non-contract Suppliers
While the September 2012 Medicare Claims Processing Manual revision coupled with the competitive bidding regulations appear to prohibit contract suppliers from utilizing upgrade ABNs for competitively bid items that are classified within a single, common HCPCS code, a non-contract supplier is permitted to utilize ABNs for competitively bid items and services within a competitive bidding area. As described within Chapter 30, Section 50.12 of the Medicare Claims Processing Manual, while a non-contract supplier is generally excluded from receiving Medicare payment for DMEPOS items delivered within a competitive bid area, “a non-contracted supplier is permitted to provide a beneficiary with an item or service listed in the Competitive Bid Area (CBA) when the supplier properly issues an ABN prior to delivery of the item or service per 42 CFR § 414.408(e)(3)(ii).”20 However, in order for an ABN to be considered valid under these circumstances, not only must the beneficiary understand the meaning of the notice, but the non-contract supplier must clearly state the reason that Medicare may or may not pay for the DMEPOS item provided to the patient.21 CMS offers the following sample wording that non-contract suppliers should utilize when delivering items under an ABN within a competitive bidding area:
Since we are not a contracted supplier, Medicare will not pay for this item. If you get this item from a contracted supplier such as ABC Medical Supplies, Medicare will pay for it.
Summary
Ultimately, contracted suppliers and non-contracted suppliers are still allowed to protect against liability by properly executing ABNs for reasons of non-medical necessity. Neither contracted suppliers nor non-contracted suppliers are required to provide a beneficiary with medically unnecessary services without cost to the beneficiary. The key is for suppliers to properly identify when equipment meets the requirements. When executed properly and in the correct circumstances, the ABN remains a beneficial tool that protects a supplier’s financial interests.
References:
1) Chapter 30, Section 40.3, Medicare Claims Processing Manual, available at www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c30.pdf.
2) Id. at Section 40.3.6.
3) Id. at 40.3.1.3.
4) See generally id. at Section 50.15.
5) 42 C.F.R. § 414.408(d) (2012).
6) Chapter 20, Section 120, Medicare Claims Processing Manual.
7) DMEPOS Competitive Bidding Program: Billing Procedures for Upgrades Fact Sheet, CMS, Dec. 2010, available at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/DME_Upgrade_Factsheet_ICN900983.pdf.
8) Id.
9) Id.
10) See Chapter 20, Section 120A, Medicare Claims Processing Manual, available at www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c20.pdf.
11) Id.
12) Chapter 30, Section 50.8, Medicare Claims Processing Manual.
13) Id.
14) Chapter 20, Section 120, Medicare Claims Processing Manual.
15) HCPCS Code Update 2013, PDAC, www.dmepdac.com/resources/articles/2012/12_17_12b.html (last visited Mar. 14, 2013).
16) Id.
17) 42 C.F.R. § 414.422(e).
18) Id. § 414.422(c).
19) 72 Fed. Reg. 17,992, 18,008 (Apr. 10, 2007).
20) Chapter 30, Section 50.12, Medicare Claims Processing Manual.
21) Id.




